Perspectives on Pain
From early-stage research to clinical practice, four experts offer their take on the potential of cannabis-based pain relief

If you conducted a straw poll on the medical indications of cannabis, pain would likely be at the top of the list. With a relatively solid safety profile, legalization advocates claim that cannabis-based treatments may be a magic bullet for the chronic pain that plagues as many as 1 in 5 Americans – and thus one answer to the country’s deadly opioid epidemic. Notably, an estimated 67 percent of US cannabis prescriptions are already for chronic pain relief (1).
But beyond the anecdotes and hyperbole, there is mixed evidence for the efficacy of cannabinoids in the treatment of pain (2, 3) – perhaps unsurprising given the huge range of causes and types of pain. We spoke with four experts working across the spectrum of pain research to get a clearer idea of the state of the field – from biologists shedding light on the role of the endocannabinoid system in pain and inflammation, through to doctors running (tightly-regulated) clinical trials and assessing the impact on their patients.

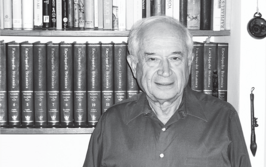
The Cell Biologist
With E. Alfonso Romero-Sandoval, Associate Professor of Anesthesiology at Wake Forest School of Medicine, Wake Forest University, North Carolina, USA.
What is the focus of your research?
We use animal, cellular and molecular models to better understand whether engaging the endocannabinoid system is beneficial in conditions causing pain or inflammation (4, 5). We investigate synthetic cannabinoid molecules selected to specifically target cannabinoid receptors found on immune cells (rather than neuronal cells) and help damp down excessive inflammatory processes, while avoiding psychotropic effects. We use models that mimic the effects of cannabinoids applied topically (through the skin), assessing their impact on skin cell function under inflammatory conditions. Our work is a long way from the clinic, but our initial results have been promising.
What do we already know about cannabinoids and pain?
Not enough! Research efforts so far have focused on enhancing the activity of endocannabinoids to reduce pain signaling. This has proven challenging – for example, some components of the system seem to attenuate the inflammatory processes, but we do not know whether this is clinically relevant. Nevertheless, when the whole cannabis plant is used, particularly when inhaled, some patients suffering from chronic neuropathic pain report partial relief (6). Our current drugs to treat neuropathic pain (pain caused by alterations in the nervous system) are only partially effective and only in a portion of patients so any new therapeutic options would be exciting.
The evidence suggests that THC is necessary to induce an effect in these patients. Interestingly, the concentrations of THC required are rather small – in the order of 5 percent or less, in some cases up to 10 percent, but certainly not higher. By contrast, cannabis used recreationally is highly potent (> 15 percent THC).
So far, we do not have any quality scientific evidence that CBD is helpful for pain conditions. The fact that CBD does not produce intoxicating effects (in contrast to THC) has created the false perspective that it is the “medicinal” cannabinoid. As a result, it has been highly marketed for multiple conditions for which there is no clinical evidence that it is useful.. We need to have more studies on CBD to better understand the risks and real potential. CBD has proven to be effective in patients with specific severe epileptic syndromes that do not respond to classic treatments. We do not have that evidence for any other condition, including pain.
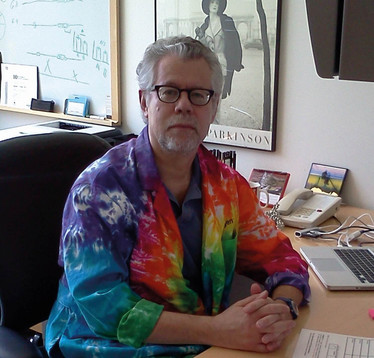
The Neuropharmacologist
With Richard J Miller, Professor of Pharmacology and Psychiatry and Behavioral Sciences at the Feinberg School of Medicine, Northwestern University, Illinois, USA.
Tell me about your background…
My work is focused on understanding how drugs interact with the nervous system. Over the years, I’ve worked on a wide variety of drugs and conditions; more recently, I’ve become involved in several projects that are focused on pain and the drugs used to treat it, including cannabis – a decision that has emerged naturally from the growing scientific and societal interest in the drug.
People have been using cannabis for thousands of years and have long remarked on its medicinal properties, including pain relief. Up until the 19th century it was freely available at pharmacies, and the idea that it should be an illegal substance only really surfaced in the 1930s, driven by political considerations. Now that we are moving away from prohibition, we are rediscovering the plant as a medicine. The difference now is that we have much more sophisticated technology, which allows scientists to evaluate claims about its efficacy.
How do pain and cannabis intersect?
There are cannabinoid receptors – specifically CB1 receptors, which bind THC – that are expressed in neurons responsible for sensing pain in the peripheral nervous system. CB1 receptors are also present in the central nervous system, including the neurons that decode these sensations into conscious experience (7). Given the locations of these receptors, it is not entirely surprising that their activation (by the body’s own endocannabinoids) may have something to do with pain control.
The question arises: if we introduce THC into the body, will that impact pain perception? The current evidence suggests that it does. To be sure, we need to apply the gold standard in testing drug efficacy, the clinical trial – but that’s difficult to do when the substance you want to administer is illegal in many countries and states.
What evidence do we have?
There are certainly some interesting case studies. In the UK recently, the case of Jo Cameron gained significant attention (8). Cameron has two genetic mutations that cause her to express very high levels of endocannabinoids; she is also completely unable to feel pain. Based on this and evidence from observational studies over the years, it does seem entirely possible that cannabinoids, particularly THC, could offer pain relief.
What’s next for research in this field?
It’s a very exciting time – changes in the law have led to the re-emergence of real scientific interest in the field. There is a long road ahead to develop effective, safe cannabis-based drugs but I expect to see a huge amount of new scientific evidence emerge over the next decade. Already, promising studies are being published in cancer and osteoarthritis. Eventually, I think cannabis will once again become a widely-used medicine around the world.

The Clinical Researcher
With Albert Dahan, Professor of Anesthesiology at Leiden University Medical Centre, the Netherlands, Founder and Head of the Anesthesia and Pain Research Unit at Leiden University, the Netherlands.
What is the goal of your research?
We focus on the effects and side-effects of opioids. In the US, the misuse of opiates has reached epidemic proportions. The situation here in the Netherlands is not so severe, and yet we still have what I would describe as a “silent epidemic.” We started by comparing different opioids, and once the severity and prevalence of opioid side-effects became apparent, we started to look at alternatives. That’s how we began working with medicinal cannabis – there is some evidence that cannabis may be effective for pain so we got in medical-grade cannabis growers Bedrocan and began discussions about how we might work together.
Our most recent publication (9) is the result of a rather complex pharmacokinetic and pharmacodynamic study.
Please, tell us more about that study…
We wanted to understand how cannabinoids – and in particular THC and CBD – affect pain processes. We decided to work with fibromyalgia patients because they are a large population of patients experiencing severe chronic pain. It’s a very heterogeneous group with very few treatment options. To establish whether CBD and/or THC had an impact on pain we carried out an experimental pain study, using a selection of pain tests. This is in contrast with the majority of studies on cannabis for pain, which take an observational approach.

What did you find?
Firstly, there was a huge difference in the effect of CBD and THC on pain – CBD had no analgesic effect; in contrast, THC had a powerful effect. We were surprised by this result, because many pain patients use CBD oil and report a good effect. It might be that they do not experience true pain relief, but rather an alteration in mood or quality of life. It should also be noted that this was a small study (20 patients) and we only tested a single application – one inhalation of cannabinoid extract for about five minutes, followed by five to six hours of follow-up.
What was even more significant was the observation that when you combine the two cannabinoids, CBD appeared to enhance THC uptake. We have a couple of explanations for this; we think that CBD uptake might increase flow across the blood brain barrier, thus driving uptake of THC. Alternatively, some CBD might be metabolized into THC.
Next, we will look at the interaction between cannabis and opioids to see if they might interact synergistically. You would hope to see pain relief but with reduced toxicity and side-effects, and reduced abuse potential.

The Pain Consultant
With Attam Singh, Consultant at The Medical Cannabis Clinic, London, and the London Pain Clinic, UK.
How did you get interested in medicinal cannabis?
It is an area that everybody seems to be talking about – especially doctors in the pain sector. We are dealing with a symptom that is highly subjective and that makes it difficult to measure. Often, we will hear very positive reports about a medication from patients, but when we try to transpose that into a clinical trial with a much more formalized processes and management, the results often do not match up to the expectation.
Can cannabis really be a viable therapeutic?
There are a lot of unknowns. As physicians, our first rule is to do no harm. When we try any new intervention, we are very cautious. One of the things I see from my colleagues in the pain field is a desire for more evidence. They want to be educated about cannabis and to know more about what they can prescribe. They also want to see it in action before they start prescribing. Once we start supporting the field – in meetings, in conferences, in studies and clinical trials – it should help steer us towards pioneering these treatment options.
How are you supporting research?
All of our patients at The Medical Cannabis Clinic are enrolled in clinical trials because we think it is important to get as much high-quality evidence as possible. Particularly here in the UK, there is a really big push to determine exactly what conditions these products are beneficial for. We want concrete clinical evidence – with guidelines for prescription and precaution – before we see more widespread adoption of cannabinoids as a medical treatment. I do feel that we will get there, and I think we are making a positive first step. When medical cannabis eventually takes off, I can see the market exploding into life.
- KF Boehnke et al., “Qualifying conditions of medical cannabis license holders in the United States”, Health Aff (Millwood), 38, 295 (2019). DOI:10.1377/hlthaff.2018.05266
- SM Nugent et al., “The effects of cannabis among adults with chronic pain and an overview of general harms: A systematic review”, Ann Intern Med, 167, 319 (2017). DOI: 10.7326/M17-0155
- A Blake et al., “A selective review of medical cannabis in cancer pain management”, Ann Palliat Med, 6, S215 (Suppl 2) (2017). MID: 28866904. DOI: 10.21037/apm.2017.08.05
- EA Romero-Sandoval et al., “Cannabis for chronic pain: challenges and considerations”, Pharmacotherapy, 38, 651 (2018). DOI: 10.1002/phar.2115
- EA Romero-Sandoval et al., “Cannabis and cannabinoids for chronic pain”, Curr Rheumatol Rep, 19, 67 (2017).. DOI: 10.1007/s11926-017-0693-1
- S Vučković et al., "Cannabinoids and pain: new insights from old molecules", Front Pharmacol, 9, 1259 (2018). DOI: 10.3389/fphar.2018.01259
- Z Shenglong, U Kumar., “Cannabinoid receptors and the endocannabinoid system: signaling and function in the central nervous system” Int J Mol Sci, 19, 833 (2018). DOI: 10.3390/ijms19030833
- BBC, “The woman who doesn’t feel pain”, (2019). Available at: https://bbc.in/2WoH8fy. Accessed July 18, 2019.
- T van de Donk et al., “An experimental randomized study of the analgesic effects of pharmaceutical-grade cannabis in chronic pain patients with fibromyalgia,'' Pain, 160, 860 (2019). DOI: 10.1097/j.pain.0000000000001464.
Having thrown myself into various science communication activities whilst studying science at University, I soon came to realize where my passions truly lie; outside the laboratory, telling the stories of the remarkable men and women conducting groundbreaking research. Now, at Texere, I have the opportunity to do just that.